Seminar: Detection of Semen & Seminal Fluid Stains
By: Dr. Imran Sabri
Junior Resident,
Department of Forensic Medicine and Toxicology,
JN Medical College, AMU, Aligarh.
As the number of cases of Rape are increasing day by day there is a need of detection of sperm and semen even if present in small quantity, no matter how old the stains are, we have to detect these stains precisely. For detection of sperm and semen are the most reliable marker for the investigation in cases of rape, sodomy, Bestiality, sexual murder etc. detection of sperm is an important factor in confirming sexual assaults. This paper provides a brief review and knowhow of the need for detection of sperms and semen and various methods applied for the detection with special emphasis on the current chemical tests with accurate procedures for performing these tests.
Semen is a human body fluid present in human males. It is a viscid mucilaginous fluid with faint yellow colour and characteristic odour called seminal odour.
Volume is about 3 ml per ejaculate.
No. of Spermatozoa= 50,000 to 3,50,000 per ml. (10% of SP).
It is a suspension of spermatozoa in seminal plasma.
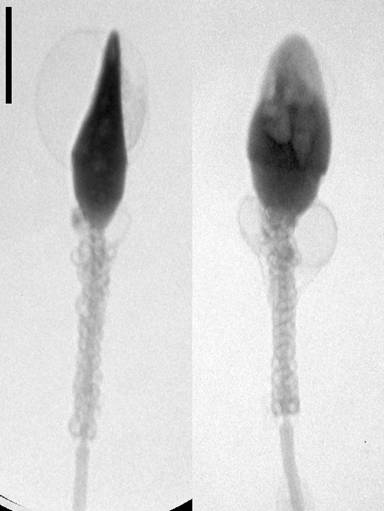
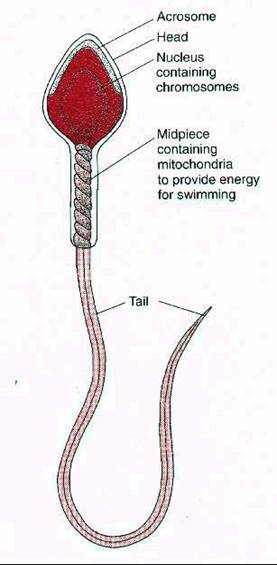

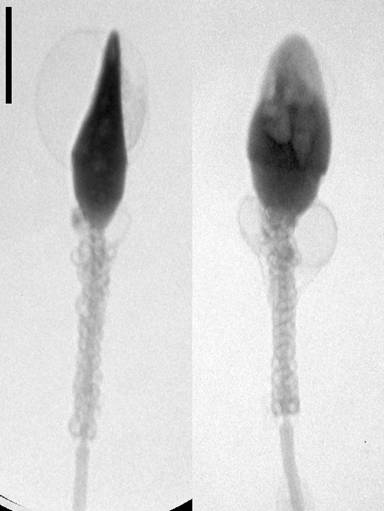
Figures 1-4 Showing Morphology of Human Sperm
Semen consist of the following
1. Spermatozoa (10%)
2. Seminal Plasma (90%)
3. Epithelial Cell (< 1%)
The Spermatozoa is produced in the testis by the process of spermatogenesis. Spermatozoa contains lipid, proteins like protamine & histone etc. and enzymes like dehydrogenises & transaminases.
The total length of spermatozoa is about 50 Microns. it consist of head and tail. The head is flat, oval shaped - 4.6 X 2.6 X 1.6 Microns. in Length Width Thickness. The nucleus, which occupies major portion of the head. The tail portion is responsible for the movement of sperm.
The seminal plasma is a mixture of secretion derived from the male accessory reproductive organs like epididymis, seminal vesicles, the prostate, vasa-deferantia, bulbourethral & urethral glands. The seminal plasma contains Citric Acid, Ascorbic Acid, Lactic Acid, Fructose, potassium Choline Phosphate, Proteases, free Amino Acids, Ergothioniene, Zinc, Calcium, Spermine, Lipids, Enzymes like Fibrinogenase, Diastase, Acid & Alkaline Phosphatase, Glysidases, a & ß Mannosidases a & ß Glucosidases, ß Givcouridases.
MEDICOLEGAL SIGNIFICANCE OF DETECTION OF SPERM & SEMEN
Rape, Sodomy (Anal intercourse), Bestiality (Sexual intercourse by a human being with a lower animal like dogs, calves, sheep etc.),In case of false Accusation by a women , Incest (Sexual intercourse in blood relation) and Sexual Murders.
Where to look for Seminal Stains
1. Clothes : Underwear, Bed sheet, Carpet, Towel, Pillow cover.
2. Body :Perineum, thigh, Vagina & pubic hair.
3. Seen of crime : On the floor or grass etc.
Method of Collection
Handling of articles bearing stains should be done very carefully to avoid damage to spermatozoa.
Vaginal / anal / penile swabs should be sent along with their smears on slides. Swabs should be taken on sterile gauze / cloth and their smears prepared on sterile slides. These should be dried in air at room temperature (37 degrees celcius) and swabs dispatched in sterile test tube and slides in clean wrappers.
Methods Applied for Detection of Seminal Stains are Classified as:
1. Physical Examination
2. Chemical Examination
3. Microscopic Examination
Physical Examination: Include Visual Examination. To naked eye seminal stains generally appear translucent or opaque spots, at times with yellowish tint and darker border depending on colour and thickness of substrata, which, if absorbent, also acquire stiffness due to dried semen. On good substrata seminal stains may appear to be fluorescent under ultraviolet light.
Chemical examination:
PH = 7.4 Alkaline.
The tests used to detect Seminal Stains are:
1. Florence Test
2. Barberio Test
3. Acid Phosphatase Test
4. LDM Isoenzyme Method
5. Acid Phosphatase Isoenzyme Test
6. Creatinine in Phosphokinase
7. Ammonium Molybdate Test (Phosphorus)
8. Semen Specific Glycoprotein (P30 ) Test
9. Enzyme-linked immunosorbent assay (ELISA), the SEMA® assay, for a seminal vesicle-specific antigen (SVSA)
Florence Test
Basis: Choline is detected in this method.
Procedure: A few drops of watery solution of the stain is extracted and taken on a slide and a drop of Florence reagent (8%) W/V solution of Iodine in water containing 5% W/V of Potassium Iodide) is poured & allowed to mix slowly under a cover slip. Dark brown crystals of choline periodide, generally needle shaped, formed with a few minutes. Non-specifics & false negative results are common.
Berberio’s Test:
Basis: Detection of Spermine
Procedure: A few drops of Berberio’s reagent when added to spermatic fluid produces crystals of sperm in picrate (needle shaped, rhombic & of yellow colour).
For various valid reasons, like non-specificity and lack of reproducibility, the florence and berberio’s tests have not been accepted universally.
ACID PHOSPHATASE SPOT TEST:
Modified Fishman and Lerner’s method. The fluid obtained after thorough maceration of a small cloth piece (about 4mm2 ) is placed in a cavity on a porcelain tile land two drops each of citrate buffer (Ph 4.9) and 1% W/V aqueous solution of disodium Phenyl phosphate are added. After 10 minutes the phenol is detected by the addition of 2 drops of phenol reagent & 2 drops of 20% W/V solution of sodium carbonate. Blue colour developed which indicates the presence of acid phosphatase.
LDH ISOENZYME METHOD
Detection of Spermatozoa
Procedure: Seminal stains are extracted with 1 ml of water. 0.25 ml of clear extract is mixed with 0.25 ml of 40% W/V of sucrose. 0.1 ml of this mixture is subjected to vertical polyacryl amide gel electrophoresis. Electrophoresis is carried out in refrigerators for 150 minutes using a current of 5 m A Isoenzyme bands are revealed by staining.
This method gives a specific biochemical detection of spermatozoa in semen in the presence of Vagtinal Fluid, Blood, Nasal Secretion, Saliva & Urine.
ACID PHOSPHATASE ISOENZYME METHOD
Procedure: Seminal stains are extracted with water and is used in polyacrylmile gel Electrphoretic method followed by staining with methyl belliferyl. Phosphate reagent enable the seminal acid phosphatase to be distinguished from that of other substance like vaginal secretions.
The method is sufficiently specific & applicable to semen derived from normal, oligospermic azoospermic & vasectemized individuals.
Advantages:
1. LDH isoenzyme is stable in stains for over 4 week.
2. Isoenzyme pattern of human is different from that of animal.
3. Positive results are obtain in large number of cases.
4. Can differentiate from vaginal secretions on pattern of bands.
CREATININE PHOSPHOKINASE:
Bases: Detection of creatinine phosphokinase. Normal seminal fluid content - 385 - 14000 U of CPK/W.
Diagnosis: >400V of CPK / ml.
Adv: Enzyme is stable & can be demonstrated in old status of six months.
CHOLINE AND SPERMINE TEST:
Bases: Unique combination of choline & spermine is present only in semen.
Liquid semen & dried seminal stains can be identified by a thin layer chromatographic Technique.
1 ML of semen present can be detected by this method.
MICROSCOPIC EXAMINATION:
The Micro Scopic detection of the Seminal stains is based in morphology of spermatozoa.
Microscopic detection of spermatozoa. Cloth pieces from different stains are taken in 0.5 ml of 0.01 N HCL in small test tubes placed in a beaker containing water. After sonication for 5 minutes the extracts and the cloth pieces are transferred to separate micro scope slides and cloth pieces delicately teased with a needle. Threads are removed and the residual liquid is gently evaporated to dryness. Residue obtained is stained haematoxylin and eosin.
Fluorescence MicroScopy:
Is also used for detection of spermatozoa. It is based on the principle that Y Chromo some is fluorescent to quinacrine. With this method it is possible to detect both intact spermatozoa as well as the disconnected heads.
Conclusion
With the above review it is quite clear that although there are so many test available for the detection of semen & sperms required to examine in cases of rape, sexual murder, unnatural, sexual offences. These tests have their won limitations advantages and disadvantages. For various valid reasons like non-specificity and lack of reproducibility the Florence and berberio’s tests have not been accepted universally apart from positive Florence test can also be obtained from other body tissue containing choline. Negative Florence may be obtained from seminal stain in case the choline content is low or in cases where the stains are decomposed. However false positive test are not obtained in cases of vaginal secretion.
Acid phosphatase of prostatic origin is also utilized for the bio-chemical detection of semen. Any interference of serum acid phosphatase caused by the admixture of blood in the seminal stains was till recently ruled out by taking - advantage of the fact, that only prostatic acid phosphatase is inhibited by 1-tartrate. This distinction, however, became invalid after the demonstration by Willott in 1972 and Davies and Wilson in 1974, that vaginal Acid phosphatase could also be inhibited by 1-tartrate. Apart from these tests other tests like Radio-immuno assay and commercial enzyme-linked immunosorbent assay (ELISA) are also available. Commercial enzyme-linked immunosorbent assay (ELISA), the SEMA® assay, for a seminal vesicle-specific antigen (SVSA) provides highly sensitive detection of semen but these tests are costly enough restricting their use for research purpose only.
The only methods among the available ones which appear to be considered as specific and unambiguous, are the microscopic or electrphoretic detection of spermatozoa in seminal stains derived from normal individuals and the electrphoretic detection of seminal Acid phosphatase in stains originating from all individuals whether normal or abnormal.
REFERENCES
1. Ricci LR, HOFFMAN sa. Prostatic acid phosphatase and sperm in the postcoital vagina. Ann Emerg Med 1982; 11: 530-534
2. Davies A. Evaluation of results from tests performed on vaginal, anal and oral swabs received in casework. J Forensic Sci Soc 1977;17:127-130.
3. Haimovici F, Anderson DJ. Detection of semen in cervicovaginal secretions. J Acquir Immune Defic Syndr Hum Retrovirol 1995; 8(3): 236-238.
4. Forensic Science Research and Training Center Laboratory Division-F.B.I. Academy. Proceedings of a forensic science symposium on the analysis of sexual assault evidence, July 6-8, 1983. Washington, DC: US Government Printing Office, 1984.
5. Hooft P, Van de Voorde H. Evaluation of the modified zinc test and the acid phosphatase test as preliminary screening methods in sexual assault case material. Forensic Sci Int 1992; 53(2): 135-141.
6. Hooft P, Van de Voorde H. Interference of body products, food and products of daily life with the modified zinc test and the acid phosphatase test. Forensic Sci Int 1994; 66(3): 187-196.
7. Young WW, Bracken AC, Goddard MA, Matheson S. Sexual assault: review of a national model protocol for forensic and medical evaluation. New Hampshire Sexual Assault Medical Examination Protocol Project Committee. Obstet Gynecol 1992;80(5): 878-883.
8. Pawlowski R. Brinkmann B. Evaluation of sperm specific lactate dehydrogenase isoenzyme C4; application to semen detection in stains. Int J Legal Med 1992;105(2): 133-126.
9. Graves HCB, Sensabaugh GF, Blake ET. Postcoital detection of a male specific semen protein. N Eng1 J Med 1985; 312: 338-343.
10. Keil W, Bachus J, Troger HD. Evaluation of MHS-5 in detecting seminal fluid in vaginal swabs. Int J Legal Med 1996; 108 (4): 186-190.
11. Lolov SR, Yomtova VM, Tsankov Y, Kehayov IR, Kyurkchiev SD. An express immunological method for detection of human seminal plasma. Forensic Sci Int 1992; 54(1): 39-50.
12. Allery JP, Telmon N. Mieusset R, Blanc A, Rouge D. Cytological detection of spermatozoa: comparison of three staining methods. J Forensic Sci 2001; 46(2): 349-351.
13. Biology Methods Manual, The Metropolitan Police Forensic Science Laboratory, London, 1978.
14. Biological Methods Manual, The Metropolitan Police Forensic Science Laboratory, London 1978.
15. T. Mann, The Biochemistry of Semen and of the Male Reproductive Tract, Methuen and Co. Ltd. London, 1964.
16. S.S. Kind, Methods of Forensic Science, Vol IV, ed by AS Curry, Interscience publishers, London/New York/Sydney, 1964.
17. G.M. Willot, JFSS, 12, 363 (1972).
18. A Davies and E Wilson, FS, 3, 45,1974.
19. R Saferstein, editor, Forensic Science Handbook, Prentice Hall Inc, Eaglewood Cliffs, New Jersey, 1982. J Flaister, Medical Jurisprudence and Toxicology, E S Livingstone Ltd, Edinburgh and London, 1967. P L Kirk, Crime Investigation, 2nd edn, ed J I Thornton, John Wiley and sons Inc, New York, 1974.
20. P K Banerjee and T K Bhattacharjee, Journal of Police Science and Administration (JPSA), 3, 280 (1975).
21. L C Nickolls, The Scientific Investigations of Crimes, Butterworths & Co. Ltd, 1956.
22. R H Mokashi A G Malwankar and M S Madiwale, JIAFS 14, 1 (1975). R H Mokashi and M S Madiwale, FS, 8, 269 (1976).
23. R H Mokashi, V.M. Chitale, S K Meghal and M S Madiwale, JIAFS, 17, 41, (1978).
24. A.H. Dange and M S Madiwale, C Z India Instruments Review, (3) 2 (1978).
25. S. Sivaram and H L Bami, JFSS, 11, 187 (1971). R.H. Mokashi and M.S. Madiwale, unpublished data.
26. F.E. Camps, editor, , Gradwohl’s Legal Medicine, John Wright and Sons Ltd. Bristol, 2nd edn, 1968. L.C. Nickolls, The Scientific Investigation of Crime, Butterworths and Co. Ltd. 1956. R. Saferstein, editor, Forensic Science Handbook, Prentice Hall Inc, Englewood Cliffs, New Jersey, 1982.
27. W. Mansi, Nature, 181, 1281 (1958).
28. H. Proom, JP, 55, 419 (1943).
29. W C Boyd, Fundamentals of Immunology, Interscience Publishers Inc, New York 1947.
30. Modi's Medical Jurisprudence and Toxicology 22nd Edition
31. Parik's Textbook of Medical Jurisprudence and Toxicology
32. Dr. K.S.N. Reddy, The Essentials of Forensic Medicine and Toxicology.
33. Chen JT, Hortin GL Journal of Forensic Sciences, Volume: 45 Issue: 1 Year: 2000 Pages: 234-235